The most important specific personality disorders are identified with diagnostic criteria, and all other presentations can be diagnosed and described using the diagnosis of personality disorder–trait specified. The Alternative Model has been judged to be more clinically useful than the DSM-IV (now DSM-5 Section II) approach in the DSM-5 Field Trials and in a large national survey of psychiatrists and psychologists . The various components of the Alternative Model have been shown to be useful in planning treatment and predicting its outcome. Our expectation is that it will be easy and straightforward to use and that it will change for the better the way clinicians think about their patients with personality pathology. Nevertheless, maladaptive personality traits will be evident in many individuals seeking treatment for other mental disorders, such as anxiety, mood, or substance use. Many of the people with a substance use disorder will have antisocial personality traits; many of the people with mood disorder will have borderline personality traits.
The prevalence of personality disorders within clinical settings is estimated to be well above 50% . As many as 60% of inpatients within some clinical settings are diagnosed with borderline personality disorder . Antisocial personality disorder may be diagnosed in as many as 50% of inmates within a correctional setting (Hare et al., 2012). It is estimated that 10% to 15% of the general population meets criteria for at least one of the 10 DSM-IV-TR personality disorders , and quite a few more individuals are likely to have maladaptive personality traits not covered by one of the 10 DSM-5 diagnoses. It is unclear why specific and explicit treatment manuals have not been developed for the other personality disorders.
This may reflect a regrettable assumption that personality disorders are unresponsive to treatment. As noted earlier, each DSM-5 disorder is a heterogeneous constellation of maladaptive personality traits. In fact, a person can meet diagnostic criteria for the antisocial, borderline, schizoid, schizotypal, narcissistic, and avoidant personality disorders and yet have only one diagnostic criterion in common.
For example, only five of nine features are necessary for the diagnosis of borderline personality disorder; therefore, two persons can meet criteria for this disorder and yet have only one feature in common. In addition, patients meeting diagnostic criteria for one personality disorder will often meet diagnostic criteria for another. In their developmental considerations for the new DSM system Tackett and colleagues describe a life span perspective of personality pathology from early childhood to later life.
In spite of the reluctance of many clinicians to use the diagnosis before the age of 18, there is a constantly growing body of evidence that PDs can be diagnosed already in adolescence [4–6]. Personality pathology seems to be highest before the age of 20, with a decline of most of the pathological features over time . The diagnostic criteria of both, ICD-10 and DSM-IV-TR, define personality disorders to begin in childhood or adolescence.
If symptoms of Borderline Personality Disorder are assessed already in early adolescence , the prevalence rate of BPD in an epidemiological sample of 11 year old children was 3.2%. Reliability, validity, and temporal stability of BPD-diagnoses in adolescents are similar to those in adulthood . The third step in the assessment is to apply the A and B criteria for the six specific disorders included the Alternative Model. The A criteria refer to impairments in personality functioning characteristic of each personality disorder and the B criteria refer to specific personality disorder trait manifestations.
Patients who meet criteria A and B for a specific personality disorder may be given a "provisional diagnosis" of that personality disorder . Patients who do not meet the criteria for a specific personality disorder may qualify for a diagnosis of personality disorder–trait specified if they have moderate or greater impairment in personality functioning and one or more pathological personality traits . Figure 1 illustrates a stepwise approach to assessing personality disorder.
These impairments are measured in combination on a single 5-point scale of severity, the Level of Personality Functioning Scale (see DSM-5, pp. 775–778). Research indicates that generalized severity of personality psychopathology is the most important single predictor of concurrent and prospective dysfunction . It is widely agreed (e.g., 4–8) that assessment of severity is essential to any dimensional system for personality psychopathology. The assessment of personality functioning goes back to the psychoanalytic concept of personality structure.
Kernberg was the first to combine the domains of identity, psychic defences, and reality testing to distinguish different levels of personality functioning or – in his terms – level of personality organization (i.e. neurotic, borderline, & psychotic). In Kernberg's view, the core pathology of patients with borderline and other severe personality disorders can be found in an impairment of their identity integration, what he called identity diffusion. Clinically, this state of identity diffusion leads to severe difficulties in describing oneself and others as well as problems in developing a sense of self with attitudes, interests, and life goals that are stable and reliable over time. Another consequence of identity diffusion occurs in the realm of interpersonal relationships.
Due to their fragmented representations of others, borderline patients are characterized by an impaired ability to mentalize, to empathize, and to build up and rely on stable relationships. Particularly intimate relationships are burdened by frequently changing self-states and either idealized or devaluated views of the partner . The current study aims to improve knowledge about the relationship between pathological personality traits and their corresponding personality types. The results point to some level of continuity between the two models when the variables were treated as dimensional. Contrariwise, there is a lack of strong scientific evidence to justify the maintenance of the categorical approach. We recommend the exclusion of the categorical approach from personality disorder diagnosis systems.
An "Alternative DSM-5 Model for Personality Disorders" was published in Section III ("Emerging Measures and Models") of the manual. The changes that were intended to be made in the personality disorders diagnoses in comparison to DSM-IV were remarkable and covered many areas. However, these changes have been moved to an appendix, the so called Section III of the DSM-5. In comparison to a single diagnosis the amount of information that is given within the complete diagnostic procedure of this newly proposed classification system is enormous, what is demonstrated with two cases examples of a 17 year old girl and a 15 year old boy. The diagnosis of the girl in the first case vignette would be "dependent PD" in DSM-IV-TR and DSM-5.
In the alternative model of the DSM-5 system there are four stages of assessment instead. First, it can be stated that the girl suffers from substantial personality impairment. Second, the level of impairment in self and interpersonal functioning is described as severe impairment in the four areas of identity, self-directedness, empathy and intimacy.
This broad assessment gives a lot of information that characterizes the patient in much more detail and thus can give many hints for treatment planning. Various specific types of psychotherapy focus on aspects of impairments in sense of self and in interpersonal relationships, as well as on pathological trait domains such as negative affectivity, detachment, and antagonism. For example, the goal of transference-focused therapy, an object relations model of treatment, is to change a state of identity diffusion into a more coherent identity by increasing self-reflective functioning and self-modulation of negative emotions . Mentalization-based therapy challenges automatic, distorted, and simplistic assumptions of the patient about self and others, in a fashion similar to some cognitive therapies.
Traditional cognitive-behavioral therapy uses cognitive restructuring, exposure, and intimacy skills training to decrease social anxiety and social avoidance, either in individual or group treatment . Schema-focused therapy is based on the premise that rigid patterns of avoidance and other compensatory behaviors develop to avoid triggering painful schemas about self and others. Modification of maladaptive schemas formed early in life leads to reduced expression of pathological traits (e.g., withdrawal, intimacy avoidance). According to the Alternative DSM-5 Model of Personality Disorders, Ms. B meets criteria A and B for narcissistic personality disorder, but not avoidant personality disorder, because she lacks the general trait of anxiousness.
Therefore, a diagnosis of narcissistic personality disorder can be made. Purpose of review The goal of the current paper is to review the DSM-5 Alternative Model for Personality Disorders , with particular focus on treatment of personality pathology. We briefly outline limitations of the traditional personality disorder diagnostic system, then, review differences between it and the AMPD, and how the alternative model can be applied for intervention planning. Recent findings Criterion A of the AMPD refers to the level of self and interpersonal impairment and is required for establishing the presence of a personality disorder diagnosis. Criterion B characterizes the nature of that diagnosis by virtue of maladaptive personality traits. Both criteria have been positioned as having important treatment value, particularly when considered jointly.
Several publications illustrate the utility of the AMPD for streamlining assessment, case conceptualization, and treatment. Summary The diagnosis of personality disorder with the AMPD provides information with direct utility for case conceptualization and treatment planning. In addition, we highlight limitations in the literature related to the AMPD, with directions for future research aimed at improving understanding of the utility of the AMPD. We further situate our discussion of the AMPD within a broader scientific climate with focus on improvement of both personality and non-personality diagnosis, conceptualization, and treatment.
In the revised Diagnostic and Statistical Manual DSM-5 the definition of personality disorder diagnoses has not been changed from that in the DSM-IV-TR. However, an alternative model for diagnosing personality disorders where the construct "identity" has been integrated as a central diagnostic criterion for personality disorders has been placed in section III of the manual. The alternative model's hybrid nature leads to the simultaneous use of diagnoses and the newly developed "Level of Personality Functioning-Scale" . Pathological personality traits are assessed in five broad domains which are divided into 25 trait facets. With this dimensional approach, the new classification system gives, both clinicians and researchers, the opportunity to describe the patient in much more detail than previously possible.
The relevance of identity problems in assessing and understanding personality pathology is illustrated using the new classification system applied in two case examples of adolescents with a severe personality disorder. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), provides a comprehensive framework for symptoms and classification of behavioral health conditions. However, efforts to make codependency a recognized disorder have been unsuccessful.
The latest iteration of diagnostic criteria, the DSM-5, only includes dependent personality disorder as an official diagnosis, not codependency. Note that it is not the goal of this review to evaluate evidence for these other quadrants, but they are specified for completeness and are relevant to future empirical work that seeks to test the hypotheses generated by the STAR model (Fig. 1). It is evident that all individuals have a personality, as indicated by their characteristic way of thinking, feeling, behaving, and relating to others. For some people, these traits result in a considerable degree of distress and/or impairment, constituting a personality disorder. The APA currently conceptualizes personality disorders as qualitatively distinct conditions; distinct from each other and from normal personality functioning. However, included within an appendix to DSM-5 is an alternative view that personality disorders are simply extreme and/or maladaptive variants of normal personality traits, as suggested herein.
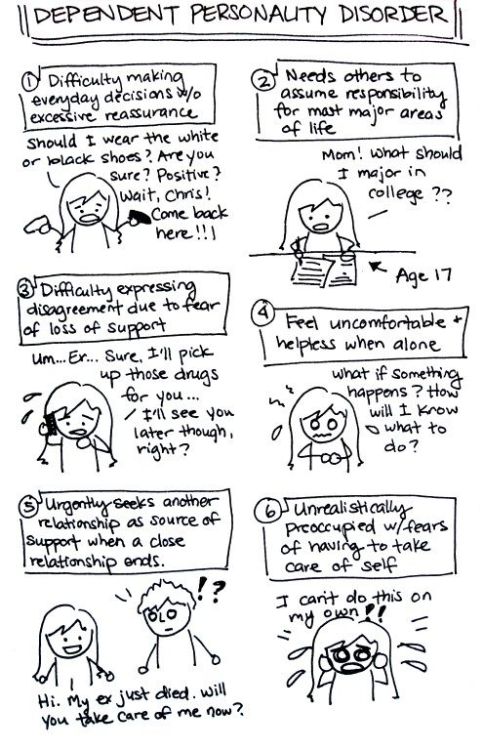
Nevertheless, many leading personality disorder researchers do not hold this view (e.g., Gunderson, 2010; Hopwood, 2011; Shedler et al., 2010). Each of the 10 DSM-5 (and DSM-IV-TR) personality disorders is a constellation of maladaptive personality traits, rather than just one particular personality trait (Lynam & Widiger, 2001). Dependent personality disorder includes submissiveness, clinging behavior, and fears of separation , for the most part a combination of traits of neuroticism and maladaptive agreeableness (e.g., gullible, guileless, meek, subservient, and self-effacing).
Antisocial personality disorder is, for the most part, a combination of traits from antagonism (e.g., dishonest, manipulative, exploitative, callous, and merciless) and low conscientiousness (e.g., irresponsible, immoral, lax, hedonistic, and rash). See the 1967 movie, Bonnie and Clyde, starring Warren Beatty, for a nice portrayal of someone with antisocial personality disorder. The Board of Trustees decided to keep the old criteria (with well-known lack of reliability and validity) despite the major revision proposed by the DSM-5 Personality Disorders Work Group. The proposed new classification system was based on 14 years of work, was more evidence-based, and with potential for greater clinical utility than DSM-IV. The major focus of the proposed revision was on the introduction of a dimensional model to the assessment and understanding of personality disorders, parallel to the dimensional models of normal personality that are widely accepted.
Since there is still a need for categorical diagnoses in our current health care system, the Work Group proposed a hybrid model of personality disorders. However, the decision of the APA Board of Trustees retains a 30 year old system that remains in substantial need of repair. People tend to seek interaction, connections, attachments, and relationships with other people. In fact, mental health is partly defined with regard to the strong emotional attachments to, and flexible interdependence on, close relationships we maintain with one another. But when interdependence becomes unbalanced to the degree that it is one-sided, it can become problematic, particularly if dependent personality disorder is involved. DPD can have a major impact on the ability to function in daily life.
For instance, society holds expectations regarding individual decisiveness, independence, and self-reliance that are dependent on age and situation, such as physical or medical issues. A person who does not meet those expectations could face difficulty functioning in school, work, and other interpersonal situations. In the interpersonal sphere, Ms. B is attuned to others' opinions of her and she is very sensitive to criticism and rejection, consistent with avoidant personality disorder. However, she is also unaware of the feelings and needs of others and underestimates how her behavior affects them, in common with narcissistic personality disorder. The latter characterization appears to fit Ms. B's interpersonal functioning better.
The A criterion for personality disorders according to the Alternative Model requires difficulties in at least two of the four areas of identity, self-direction, empathy, and intimacy. Manifested as excessive and consistently recurrent emotional distress on account of past psychological traumas. The distress did not present with daytime flashbacks or nightmares, feelings or symptoms of significant anxiety, nor panic.
It is interesting to note that despite management with medications for anti-depression treatment, the patient remained cyclically refractive, regarding her affective mood. On two occasions, when the patient initially agreed on a discharge date, on the morning of discharge, she stated, "I'm not ready. Cognitive behavioral therapy and supportive psychotherapy services were referred to follow up as an outpatient telehealth treatment plan for the patient's mental illness.
These symptoms give a picture of just how much destruction Dependent Personality Disorder can cause in an individual's life. The disorder often introduces many personal and professional difficulties. Personally, people with the disorder have a hard time forming mutual relationships that do not becoming clingy or dependent. People with the disorder often do not have relationships outside of their family.
Professionally, people with the disorder look for others to take care of them so they rarely take initiation—something that is essential in the professional world. In addition, the disorder raises people's risk of other mental illnesses, including other anxiety, depression, adjustment, and personality disorders. DSM-5 offers an alternative model of personality pathology that includes 25 traits. Although personality disorders are mostly treated with psychotherapy, the correspondence between DSM-5 traits and concepts in evidence-based psychotherapy has not yet been evaluated adequately. Suitably, schema therapy was developed for treating personality disorders, and it has achieved promising evidence. The authors examined associations between DSM-5 traits and schema therapy constructs in a mixed sample of 662 adults, including 312 clinical participants.
Associations were investigated in terms of factor loadings and regression coefficients in relation to five domains, followed by specific correlations among all constructs. The results indicated conceptually coherent associations, and 15 of 25 traits were strongly related to relevant schema therapy constructs. Conclusively, DSM-5 traits may be considered expressions of schema therapy constructs, which psychotherapists might take advantage of in terms of case formulation and targets of treatment. In turn, schema therapy constructs add theoretical understanding to DSM-5 traits. Administration of a personality questionnaire to assess pathological personality traits was performed utilizing the DSM-V personality assessment (The Personality Inventory for DSM-5 also known as PID-5 ). The personality test was performed to assess the patient's personality disorder and identify possible characteristics that align with the personality disorder identified in this case study.
PID-5 has been commonly used as a reliable instrument used to identify personality disorders. Personality pathologies seen in psychiatric patients may or may not be identifiable in the DSM-V psychiatry manual. Health anxiety disorders (e.g., hypochondriasis) are prevalent but understudied in older adults.
Existing research suggests that severe health anxiety has a late age of onset, perhaps because of comorbidity with physical health conditions that are more likely to occur with aging. Despite being under diagnosed in later life due to a lack of age-appropriate diagnostic criteria, significant positive associations with age suggest that health anxiety disorders are more prevalent in older than younger adults. Preliminary research also highlights the complexity of these disorders in older adults and the potential importance of medical morbidity as a risk factor.




















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.